Insurance Eligibility
Feature # 32744 - Service Type Level Deductible added to Eligibility Limit Payment Table calculation
Summary
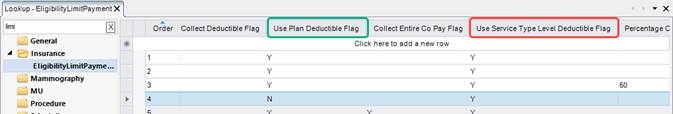
This enhancement to Insurance Eligibility updates the Eligibility Limit Payment Table with a new Use Service Type Level Deductible column. This new column in conjunction with the existing Use Plan Deductible column will provide a more enhanced level of configuration to the Eligibility workflow.
Feature Description
Previously, there was no way to configure whether to use or not use the deductible in the service type section (sometimes referred to as the “modality deductible or the “lower level deductible”).
With this change, RIS can be configured by specific carrier to either use the Plan deductible, use the Service Type Level deductible, or both.
The addition of the Use Service Type Level column introduces the following configuration scenarios:
|
Use Plan Deductible Flag |
Use Service Type Level Deductible Flag |
Scenario |
|
Y |
Y |
eRAD RIS will take the lowest listed remaining deductible. |
|
N |
Y |
eRAD RIS will use the Service Type Level deductible. |
|
Y |
N |
eRAD RIS will use the Plan Deductible. |
|
N |
N |
This configuration combination would ignore all deductibles. |
Configuration Instructions
System Administrators must complete the following actions to enable this feature:
RIS Client
Changes to EligibilityLimitPayment Lookup Table
1. Set Use Service Type Level = Y for desired carriers to ensure the service type deductible is being used.
Summary
This enhancement to Insurance Eligibility introduces configuration to reduce the pricing for a visit when the same billing code is repeated for a visit. The full price will be charged for the initial instance and repeated instances of that code will be billed at a reduced rate, according to the configuration for the payer/carrier and billing code.
Background
Previously, multiple units of the same billing code or a billing code repeated on multiple studies, such as a Procedure X (Left) and Procedure X (Right), were all billed at the same rate.
Feature Description
With this change, the sum of the costs of billing codes will depend on the configuration for that payer/carrier and billing code, allowing RIS to charge the full amount for the first occurrence of the billing code then a reduced percentage for each additional occurrence of the same code.
For example: If we have, carrier ‘6004’ (Aetna Commercial and 2 units of billing code ‘76541’ which has a normal cost of $145.99 but we only want to charge 50% of the cost of ‘abc’ for the second unit so the total cost of the ‘abc’ billing codes is only $218.99 (i.e., 145.99 + 73) instead of $291.98.
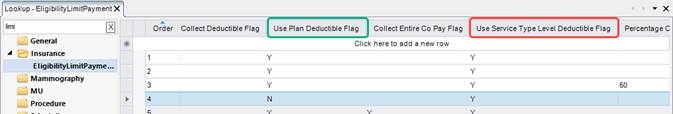
With this change, the EligibilityLimitPayment lookup table has been updated with a new Percentage Cost For Repeated Billing Codes column that reduces the cost for repeated instances of the same billing code.

Enter the percentage reduction, for example 50 for 50% reduction.
Known Limitations
While there are no Known Limitations for this feature, there is additional functionality planned for a future release that will change the implementation approach, and is expected to impact how this feature will be configured:
· Feature #30707 - Payment Rules: Restructure Payment Rules configuration table to accommodate for Billing Code, Procedure or Visit level rules
Configuration Instructions
System Administrators must complete the following actions to enable this feature:
RIS Client
Changes to EligibilityLimitPayment Lookup Table
· Configure the new Percentage Cost For Repeated Billing Codes column for each payer/carrier and billing code combination with the desired cost reduction percentage.